How Diet Can Treat Autoimmune Diseases
Oct 24, 2023As our understanding of the human body evolves, it becomes increasingly clear that the interplay between our internal systems, the external environment, and what we consume significantly influences our well-being. Among these factors, autoimmune diseases stand out as a poignant testament to the body's ability to mistakenly target itself, often leading to chronic ailments that can disrupt one's quality of life.
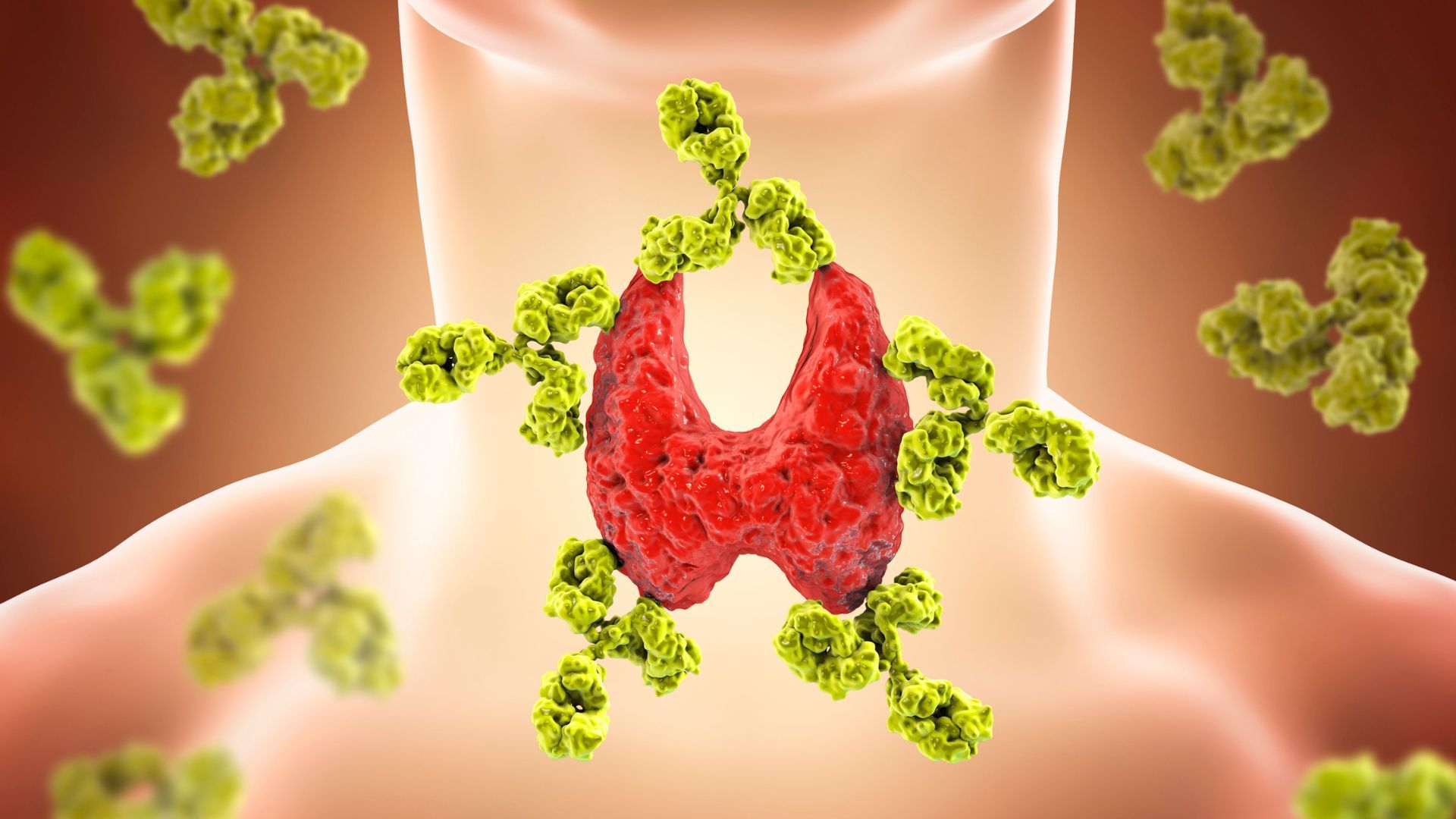
Autoimmune diseases, at their core, occur when the body's immune system, mistakenly identifies its own cells in specific tissues as threats and begins attacking them. This phenomenon can lead to a plethora of complications, ranging from skin disorders to more severe conditions affecting vital organs.
Understanding autoimmune diseases and their treatment is becoming more and more important in practice. They impact millions worldwide. As we delve deeper into the causative factors and potential remedies for these conditions, the role of nutrition emerges as a cornerstone. Through dietary adjustments and a keen understanding of how specific foods influence our immune responses, many individuals have found relief, if not total respite, from their autoimmune symptoms.
Understanding Autoimmune Diseases
Autoimmune diseases represent a broad category of disorders, each unique in its manifestation but unified by a common mechanism: the body's immune system turning against its tissues. This "self-attack" can have various origins, often influenced by a combination of genetic, environmental, and lifestyle factors. To provide a clearer picture of these conditions, let's delve into their defining characteristics, common examples, and general symptoms.
- Definition and Mechanism: At its core, an autoimmune disease arises when the immune system, which usually wards off foreign invaders such as bacteria and viruses, fails to distinguish between these invaders and the body's healthy cells. Instead, the immune system produces autoantibodies that attack healthy cells, tissues, and organs (Rose and Mackay, 2014). This misguided immune response can be localized to a specific organ or may affect the body more generally.
- Common Examples:
- Rheumatoid arthritis (RA): An autoimmune disease where the immune system attacks the joints, causing inflammation and pain (McInnes and Schett, 2011).
- Lupus: A systemic disorder affecting multiple organ systems, characterized by inflammation and damage (Tsokos, 2011).
- Celiac disease: Triggered by the ingestion of gluten in genetically predisposed individuals, it results in damage to the lining of the small intestine (Green and Cellier, 2007).
- Type 1 diabetes: The immune system attacks and destroys insulin-producing cells in the pancreas (Atkinson and Eisenbarth, 2001).
- And many others, including multiple sclerosis, psoriasis, and Graves' disease.
- Symptoms and Diagnosis: Symptoms of autoimmune diseases can vary widely depending on the specific disease and the individual. However, general symptoms often include fatigue, muscle aches, and low-grade fever. Many autoimmune diseases also have periods of remission (when symptoms fade) and flare-ups (when symptoms return or intensify). Diagnosing these conditions can be a challenge, often requiring a combination of medical history assessments, physical exams, and specific blood tests (American Autoimmune Related Diseases Association, n.d.).
Nutrition and the Immune System: A Brief Overview
Our daily diet plays a foundational role in determining overall health, but its influence on the immune system is particularly profound. Understanding the relationship between nutrition and immune function is essential for gauging the impact of dietary choices on autoimmune diseases.
The Significance of Nutrition in Health:
Nutrition is a cornerstone of health, influencing various physiological functions, from energy production to cellular repair. Proper nutrition ensures the optimal function of the body's systems and helps in disease prevention and recovery (Shanahan and Shanahan, 2011).
The Interplay Between Nutrition and Immune Function:
The immune system, in its fight against pathogens and harmful agents, relies heavily on nutrients derived from our diet. Specific vitamins, minerals, and other bioactive compounds can either strengthen or weaken immune responses:
- Vitamins: Vitamin C, for instance, is known for its role in bolstering the immune system, aiding in white blood cell function, and enhancing barrier functions (Carr and Maggini, 2017). Similarly, Vitamin D has been recognized for its ability to modulate both innate and adaptive immune responses (Aranow, 2011).
- Minerals: Zinc, selenium, and iron play crucial roles in immune cell growth, function, and signaling (Wintergerst, Maggini, and Hornig, 2007).
- Bioactive compounds: Phytochemicals and antioxidants found in various plants can influence immune responses by combating oxidative stress and modulating inflammation (Biesalski, 2007).
Impacts of Malnutrition:
Insufficient intake of essential nutrients can impair immune function. Both undernutrition and overnutrition can lead to an increased susceptibility to infections, slow recovery from illness, and potentially contribute to the onset of autoimmune reactions (Chandra, 1997).
The Gut-Immune Connection
The human gastrointestinal system, more commonly known as the gut, plays a pivotal role in our overall health. Often referred to as the body's "second brain," the gut is not just responsible for digestion but also serves as the home to a complex community of trillions of microorganisms, collectively known as the gut microbiota. The intricate relationship between the gut, its resident microbiota, and the immune system has emerged as a significant area of research, especially in understanding autoimmune diseases.
The Gut Microbiota – A Brief Overview:
Our gut hosts a diverse array of bacteria, fungi, viruses, and other microorganisms. These microbial communities play a role in nutrient absorption, synthesis of vitamins, and protection against harmful pathogens. A balanced gut microbiota promotes intestinal health and, by extension, impacts the function of various other bodily systems (Hill et al., 2014).
Linking Gut Health and Immune Responses:
The gut is intrinsically tied to the immune system in several ways:
- Intestinal Barrier Function: The gut lining acts as a protective barrier, preventing the entry of pathogens while allowing nutrient absorption. A compromised barrier, often termed "leaky gut," can lead to increased permeability, allowing harmful agents and particles to enter the bloodstream, triggering immune responses (Bischoff et al., 2014).
- Microbial Regulation of Immunity: Beneficial gut microbes can influence the immune system by regulating the balance of pro-inflammatory and anti-inflammatory immune cells. Dysbiosis, or an imbalance in the microbial community, can skew this balance, potentially contributing to autoimmune reactions (Belkaid and Hand, 2014).
Diet's Role in Shaping Gut Health:
Dietary choices directly influence the composition and function of the gut microbiota. Diets rich in fiber, fermented foods, and diverse plant-based foods promote a healthy microbial balance, whereas diets high in processed foods, sugars, and certain fats can foster dysbiosis (David et al., 2014).
Gut Health and Autoimmune Diseases:
An increasing body of research suggests that alterations in gut microbiota composition can be linked to various autoimmune diseases. For instance, individuals with rheumatoid arthritis or multiple sclerosis have shown distinct gut microbial profiles compared to healthy counterparts (Ma et al., 2017; Jangi et al., 2016).
In essence, the gut stands as a vital crossroad between nutrition, microbiota, and immunity. Prioritizing gut health through informed dietary choices may offer a promising avenue for managing and potentially preventing autoimmune conditions.
Dietary Strategies for Managing Autoimmune Diseases
Given the increasing recognition of the role of nutrition in influencing immune function and its possible impact on autoimmune diseases, dietary interventions have become a promising strategy in their management. While no one-size-fits-all approach exists, certain evidence-based dietary practices have shown potential in ameliorating autoimmune symptoms and improving overall health.
Anti-inflammatory Diets:
Inflammation is a hallmark of autoimmune diseases. Adopting diets that emphasize anti-inflammatory foods can be beneficial:
- Foods to Emphasize: Fatty fish rich in omega-3s (e.g., salmon, mackerel, sardines), colorful fruits and vegetables, nuts, seeds, and whole grains (Gioxari, Kaliora, Marantidou and Dedoussis, 2018).
- Foods to Limit: Processed foods, refined sugars, and unhealthy fats, which can exacerbate inflammation (Minihane et al., 2015).
Gluten-Free and Casein-Free Diets:
For certain individuals, especially those with celiac disease or gluten sensitivity, removing gluten from the diet is imperative. Some autoimmune patients also report benefits from eliminating casein, a protein found in dairy (Lionetti et al., 2015).
The Autoimmune Protocol (AIP):
A more restrictive approach, the AIP eliminates grains, legumes, dairy, processed foods, and certain vegetable oils. It emphasizes nutrient-dense vegetables, lean proteins, and healthy fats. Initial studies suggest its potential in managing conditions like inflammatory bowel disease (Konijeti et al., 2017).
Gut-Health Promoting Diets:
Given the gut-immune connection, diets that promote a balanced gut microbiota can be beneficial. This might include probiotic-rich foods (e.g., yogurt, kefir, sauerkraut), prebiotic foods (e.g., garlic, onions, asparagus), and a diverse range of plant-based foods (Valdes, Walter and Segal, 2018).
Vitamin and Mineral Supplementation:
Ensuring adequate intake of specific vitamins and minerals, such as vitamin D, zinc, and selenium, can be crucial, especially if deficiencies are identified. Always consult with a healthcare professional before starting any supplementation (Mora, Iwata and von Andrian, 2008).
Conclusion
Autoimmune diseases, marked by the body's immune system mistakenly targeting its own tissues, present a complex health challenge. As we've explored, nutrition plays an influential role in both the development and management of these conditions. The interconnectedness of the gut, immune system, and diet underscores the significance of dietary choices in influencing disease progression and symptom manifestation.
Dietary interventions, from anti-inflammatory diets to more specialized protocols like the Autoimmune Protocol, have shown potential in aiding the management of autoimmune conditions. These strategies, while not a panacea, provide patients with a proactive way to influence their health. By fostering a balanced gut microbiota and minimizing inflammatory triggers, nutrition can be a powerful ally in the battle against autoimmunity.
However, it's paramount to approach dietary changes with a sense of individuality and caution. What works for one person may not work for another.
In conclusion, as the field of nutrition science continues to evolve, our understanding of the intricate dance between diet, the gut, and autoimmunity will undoubtedly deepen. Harnessing the power of nutrition, backed by evidence-based knowledge, offers hope and a proactive approach to those navigating the challenges of autoimmune diseases.
References
American Autoimmune Related Diseases Association, n.d. Autoimmune Disease List. Available at: [Website link].
Aranow, C., 2011. Vitamin D and the immune system. Journal of Investigative Medicine, 59(6), pp.881-886.
Atkinson, M.A. and Eisenbarth, G.S., 2001. Type 1 diabetes: new perspectives on disease pathogenesis and treatment. The Lancet, 358(9277), pp.221-229.
Belkaid, Y. and Hand, T.W., 2014. Role of the microbiota in immunity and inflammation. Cell, 157(1), pp.121-141.
Biesalski, H.K., 2007. Polyphenols and inflammation: Basic interactions. Current Opinion in Clinical Nutrition & Metabolic Care, 10(6), pp.724-728.
Bischoff, S.C., Barbara, G., Buurman, W., Ockhuizen, T., Schulzke, J.D., Serino, M., Tilg, H., Watson, A. and Wells, J.M., 2014. Intestinal permeability – a new target for disease prevention and therapy. BMC Gastroenterology, 14(1), p.189.
Carr, A.C. and Maggini, S., 2017. Vitamin C and immune function. Nutrients, 9(11), p.1211.
Chandra, R.K., 1997. Nutrition and the immune system: an introduction. The American Journal of Clinical Nutrition, 66(2), pp.460S-463S.
David, L.A., Maurice, C.F., Carmody, R.N., Gootenberg, D.B., Button, J.E., Wolfe, B.E., Ling, A.V., Devlin, A.S., Varma, Y., Fischbach, M.A., Biddinger, S.B., Dutton, R.J. and Turnbaugh, P.J., 2014. Diet rapidly and reproducibly alters the human gut microbiome. Nature, 505(7484), pp.559-563.
Gioxari, A., Kaliora, A.C., Marantidou, F. and Dedoussis, G.V., 2018. Intake of ω-3 polyunsaturated fatty acids in patients with rheumatoid arthritis: A systematic review and meta-analysis. Nutrition, 45, pp.114-124.e4.
Green, P.H. and Cellier, C., 2007. Celiac disease. New England Journal of Medicine, 357(17), pp.1731-1743.
Hill, C., Guarner, F., Reid, G., Gibson, G.R., Merenstein, D.J., Pot, B., Morelli, L., Canani, R.B., Flint, H.J., Salminen, S., Calder, P.C. and Sanders, M.E., 2014. Expert consensus document: The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nature Reviews Gastroenterology & Hepatology, 11(8), pp.506-514.
Jangi, S., Gandhi, R., Cox, L.M., Li, N., von Glehn, F., Yan, R., Patel, B., Mazzola, M.A., Liu, S., Glanz, B.L., Cook, S., Tankou, S., Stuart, F., Melo, K., Nejad, P., Smith, K., Topçuolu, B.D., Holden, J., Kivisäkk, P., Chitnis, T., De Jager, P.L., Quintana, F.J., Gerber, G.K., Bry, L. and Weiner, H.L., 2016. Alterations of the human gut microbiome in multiple sclerosis. Nature Communications, 7, p.12015.
Konijeti, G.G., Kim, N., Lewis, J.D., Groven, S., Chandrasekaran, A., Grandhe, S., Diamant, C., Singh, E., Oliveira, G., Wang, X., Molparia, B. and Torkamani, A., 2017. Efficacy of the autoimmune protocol diet for inflammatory bowel disease. Inflammatory Bowel Diseases, 23(11), pp.2054-2060.
Lionetti, E., Pulvirenti, A., Vallorani, M., Catassi, G., Verma, A.K. and Gatti, S., 2015. Re-challenge Studies in Non-celiac Gluten Sensitivity: A Systematic Review and Meta-Analysis. Frontiers in Physiology, 6, p.346.
Ma, Y., Zhang, F. and Li, W., 2017. Gut microbiota and rheumatoid arthritis: insights, prospects, and challenges. Frontiers in Microbiology, 8, p.360.
McInnes, I.B. and Schett, G., 2011. The pathogenesis of rheumatoid arthritis. New England Journal of Medicine, 365(23), pp.2205-2219.
Minihane, A.M., Vinoy, S., Russell, W.R., Baka, A., Roche, H.M., Tuohy, K.M., Teeling, J.L., Blaak, E.E., Fenech, M., Vauzour, D., McArdle, H.J., Kremer, B.H., Sterkman, L., Vafeiadou, K., Benedetti, M.M., Williams, C.M. and Calder, P.C., 2015. Low-grade inflammation, diet composition and health: current research evidence and its translation. The British Journal of Nutrition, 114(7), pp.999-1012.
Mora, J.R., Iwata, M. and von Andrian, U.H., 2008. Vitamin effects on the immune system: vitamins A and D take centre stage. Nature Reviews Immunology, 8(9), pp.685-698.
Rose, N.R. and Mackay, I.R., 2014. The autoimmune diseases. Elsevier.
Shanahan, C. and Shanahan, L., 2011. Deep Nutrition: Why Your Genes Need Traditional Food. Big Box Books.
Tsokos, G.C., 2011. Systemic lupus erythematosus. New England Journal of Medicine, 365(22), pp.2110-2121.
Valdes, A.M., Walter, J. and Segal, E., 2018. Role of the gut microbiota in nutrition and health. BMJ, p.k2179.
Wintergerst, E.S., Maggini, S. and Hornig, D.H., 2007. Immune-enhancing role of vitamin C and zinc and effect on clinical conditions. Annals of Nutrition & Metabolism, 50(2), pp.85-94.

